Introduction
Simple and easy-to-use tools can bring surprising insights and results. Most healthcare professionals, especially safety and quality officers, are familiar with and use them during their day-to-day work. Yes, we are talking about essential patient safety tools and techniques that you use to ensure the delivery of safe and reliable care. These tools are indispensable for safety and quality management in healthcare.
This blog article looks at 9 essential patient safety tools that are commonly used in hospitals and other healthcare settings. Most of the tools are easy to use and practical hands-on techniques. They are effective and practical applications for front-line healthcare workers to improve patient safety systems and processes.
You will find a brief description of each of the tools, when to use them, how they work and in what way they help to improve patient safety. Downloadable templates are provided in Patient Safety Essentials Toolkit for quick reference.
Table of Contents
Essential Patient Safety Tools and Techniques
1. Daily Huddle
A huddle is a short briefing or meeting for 10 minutes or less involving care team members, usually held at the start of each workday or shift. A daily huddle gives teams a way to focus on care coordination, identify potential or existing safety issues and flag concerns. Huddles provide the opportunity for team members to look back and review the previous day’s work and to look ahead to flag safety issues and other concerns for patients for the day.
Daily huddle is an effective and efficient way for healthcare teams to review performance, share information and enhance team communication. While the typical huddles focus on operational issues such as handovers at shift changes, this tool is also designed to focus on patient safety and quality performance. It engages teams to review standard work such as checklists, updates specific quality and safety initiatives that affect daily work and identifies issues that need escalation.
Daily huddles help to build a culture of safety and teamwork among healthcare professionals. Significantly, huddles help nurses prioritize patient care and manage patient safety proactively.
2. SBAR (Situation-Background-Assessment-Recommendation)
SBAR is an easy-to-use, structured form of communication technique that enables information to be transferred accurately between care teams. It is widely used to enhance patient safety by reducing the risk of miscommunication and promoting a common framework for sharing information among healthcare team members.
Here is how SBAR can help you:
- It helps prevent breakdowns in verbal and written communications by providing a common framework for communication during patient handovers, critical exchange of information, situations requiring escalation, and incident reporting.
- It improves the effectiveness in communication across different disciplines and between different levels of staff by building a common language for communicating critical events and reducing communication barriers.
- It encourages staff to think and convey information clearly and avoid being vague in giving information.
- It makes handovers quicker and more effective, thereby saving more time for clinical care.
How does SBAR work?
The SBAR consists of four standardized stages that help staff to anticipate the information needed by colleagues and formulate important communications with the right level of details.
| Stages | Details |
| Situation | This is a brief and concise statement that describes the current situation or the reason for the communication. It provides an overview of what is happening with the patient. |
| Background | This section provides contextual and relevant information about the patient’s medical history, status, or relevant background information. It helps the recipient of the information understand the patient’s background and any factors that might be contributing to the current situation. |
| Assessment | This is the analysis or evaluation of the healthcare provider’s assessment of the patient’s current condition. It includes key clinical findings such as vital signs, lab results, or physical examination findings. |
| Recommendation | This section includes the specific actions or interventions suggested based on the assessment. It provides a clear direction or plan for the recipient of the information in taking the next steps in the patient’s care. |
3. ASK ME 3
Clear communication between healthcare providers and patients/caregivers is important for keeping patients healthy and safe. Ask Me 3 is an educational program developed by NPSF (and is licensed by Institute for Healthcare Improvement) to educate patients and families to ask three questions of their care providers. The simple questions are designed to help the patients and families better understand their health conditions and what they need to do to stay healthy.
The concept is simple: asking questions empowers patients. The three questions that patients should ask each time they have an appointment or hospitalization are:
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
Patients are sometimes reluctant or unaware to ask questions. By creating an environment where questions are encouraged, patients are more likely to be active participants in their health care, make less mistakes, have positive outcomes, and increase patient satisfaction. Healthcare providers should engage patients and families in discussing these questions.
4. 5 Whys
The 5 Whys is a problem-solving technique that originated from the Toyota Production System and is often used in quality management and process improvement. The goal of the technique is to identify the root cause of a problem by asking “why” repeatedly until the underlying cause is revealed.
The “5 Whys” technique encourages a systematic and thorough analysis of a problem, helping teams to move beyond addressing symptoms and focus on addressing the root causes. It promotes a more proactive and preventive approach to problem-solving. It’s important to note that the number of “Whys” may vary depending on the complexity of the problem.
Here’s how the 5 Whys process typically works:
Process | Details |
Identify the Problem | Start by clearly defining the problem or issue you want to address. Be specific and focus on one problem at a time. Begin by asking why the problem occurred. After each answer, ask “why” again, based on the previous response. Repeat this process at least five times to get to the root cause of the problem or continue this process until you reach a point where further questioning doesn’t provide meaningful insights. |
Reach the Root Cause | By asking “why” multiple times, you gradually move from the symptoms of the problem to its underlying causes. The last “why” should ideally lead you to the root cause of the issue. Once you’ve identified the root cause, you can develop and implement corrective actions to address it. |
Prevent Recurrence / Implement Solutions | Once you have identified the root cause, you can develop and implement solutions to address it. Consider additional measures to prevent the problem from recurring. This might involve changes to processes, training, or ongoing monitoring to ensure the effectiveness of the corrective actions. |
The 5 Whys technique is a simple yet powerful tool for problem-solving. It encourages a deeper understanding of issues and promotes a proactive approach to addressing the fundamental causes of problems.
5. Ishikawa Diagram / Cause and Effect Diagram (Fishbone)
 Cause and Effect Diagram is also known as Ishikawa Diagram or Fishbone Diagram. This tool helps your team to work through the possible underlying contributing factors of a problem and sort the factors into a few categories. The analysis enables your team to create insights into the problem and start to consider possible improvements or solutions.
Cause and Effect Diagram is also known as Ishikawa Diagram or Fishbone Diagram. This tool helps your team to work through the possible underlying contributing factors of a problem and sort the factors into a few categories. The analysis enables your team to create insights into the problem and start to consider possible improvements or solutions.
Fishbone Diagram is a commonly used Root Cause Analysis (RCA) tool to determine why a particular problem is occurring. It helps you to identify a wide range of possible contributing factors – not just the obvious most.
This tool graphically displays the relationship of the causes to the effect or outcome. It can also be used in identifying areas for improvement.
Causes are typically grouped under 6 categories, namely Manpower, Methods, Materials, Machine, Measurement and Mother Nature. The London Protocol identifies 7 categories of contributing factors, namely Patient Factor, Individual/Staff Factor, Team Factor, Work & Care Environment Factor, Organizational Factor, Task & Technology Factor, and External Factor.
6. FMEA (Failure Modes and Effect Analysis)
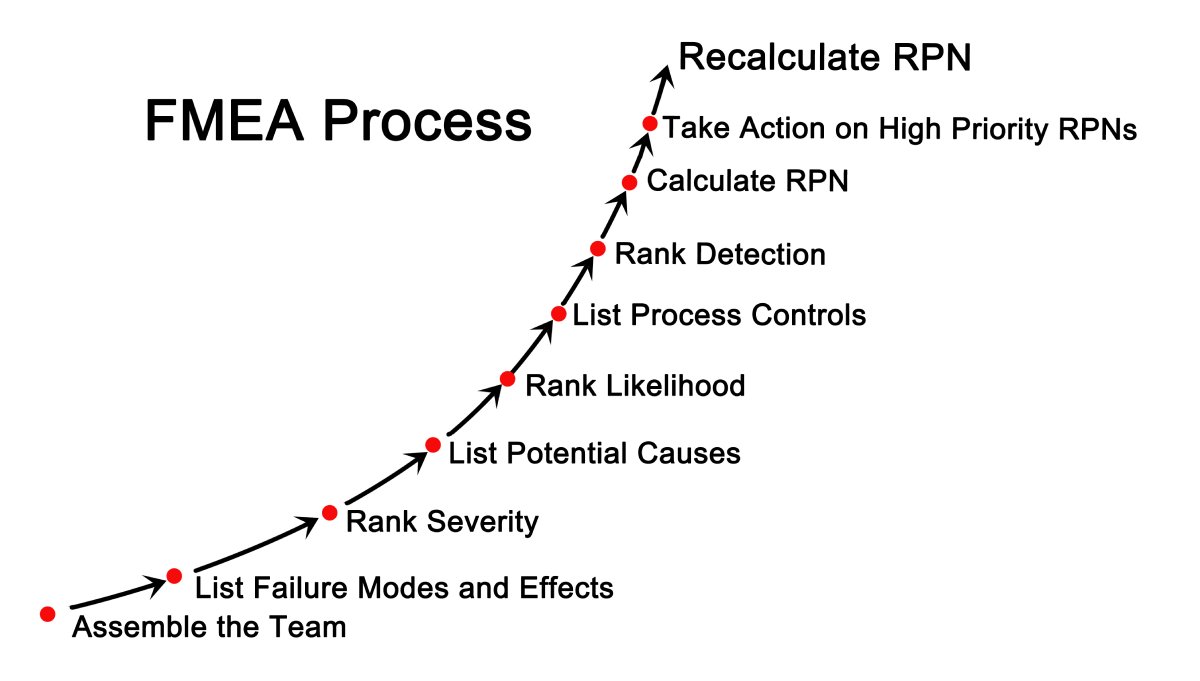 FMEA is a technique for conducting a systematic analysis of processes or products to identify and prevent any problems before they occur. It prompts your team to proactively review and evaluate what could go wrong (failure mode), why failures happen (failure causes), and the consequence of failure (failure effect). Improvement plans can then be carried out to prevent those failures.
FMEA is a technique for conducting a systematic analysis of processes or products to identify and prevent any problems before they occur. It prompts your team to proactively review and evaluate what could go wrong (failure mode), why failures happen (failure causes), and the consequence of failure (failure effect). Improvement plans can then be carried out to prevent those failures.
The focus of FMEA is to proactively identify potential risks or failure points and their impact, prevent failures and make the system more resilient. The emphasis is on preventing or reducing harm to patients or staff. FMEA is particularly useful in evaluating a new process prior to its implementation, and in assessing and managing the impact of the proposed change to existing processes. Healthcare organizations should apply FMEA to access new services and procedures before implementing them.
In an FMEA exercise, the team comprising representatives from all areas of the process under review convenes to discuss and predict where, how, and to what extent the system might fail. Failure mode with high Risk Profile Number (RPN) are probably the most important parts of the process on which to focus improvement efforts. Team members will then prioritize and work together to devise improvement plans to prevent those failures — especially failures that are likely to occur or would cause severe harm to patients or staff.
7. Action Hierarchy (part of RCA2)
A critical step in the RCA process is the identification and implementation of actions to address system vulnerabilities that have been identified. Investigation teams should design actions to prevent incidents from recurring. If that is not possible, reduce the probability and severity of harm to the patient should it occur. Studies have shown that the lack of emphasis on actions is one of the main reasons for RCAs not yielding the desired results.
The Concept of RCA2
To improve the effectiveness of RCA, the National Patient Safety Foundation (NPSF) of the US introduced the concept of RCA2 (RCA and Action or RCA squared) in 2015. RCA2 methodology emphasizes actions after the analysis is done, as the ultimate objective of RCA is to prevent future harm by implementing corrective and preventive actions.
Action Hierarchy
Action Hierarchy is a tool that will assist investigation teams in identifying stronger actions that provide effective and sustained system improvement. It is recommended that investigation teams should identify at least one stronger or intermediate strength action for each RCA.
Actions | Details |
Stronger Actions | Likely to eliminate or greatly reduce recurrence of event. |
Intermediate Actions | May help to control the event identified. |
Weak Actions | Less likely to be effective when used alone. |
All levels of action are important. Stronger actions are generally less reliant on humans, and vice versa. Weaker actions may be important to support stronger actions. Weaker actions can also be used as temporary measures until stronger actions can be implemented. Examples of stronger actions are major renovation of a nursing unit to move the nursing station to a more central location for better visibility and accessibility by nurses, staff, and patients/families.
8. Flowchart
Also known as a Process Map, flowchart is a visual representation of the sequence of steps in a process. Having a clear understanding of your current process and how it works is an important first step in identifying and developing improvement plans.
The visual representation of current processes helps teams to better focus to identify problems or bottlenecks. Steps that do not add value, causing breakdowns in communication or are unnecessary, can become more apparent when viewing in a flowchart. Such analysis can be the basis for implementing improvement plans.
For example, flowcharts can help to find one or multiple sources of a problem or examine the handoff that occurs in a process. At times, it is being used to identify personnel, groups, or entire departments that are responsible for processes or tasks.
To create a flowchart, your team will brainstorm all the steps in the current process. Each process step is written in a box. In addition to the steps themselves, use a diamond shape to indicate points in the process where a decision needs to be made. For decision steps, your team writes a yes/no question. Then use lines to show the connections between the boxes and diamonds.
9. Pareto Chart
 The Pareto principle, commonly known as the “20/80 rule”, is an important quality tool for safety and process improvement. According to the Pareto principle”, in any group of factors that contribute to an overall effect, roughly 80% of the effect comes from 20% of the causes.
The Pareto principle, commonly known as the “20/80 rule”, is an important quality tool for safety and process improvement. According to the Pareto principle”, in any group of factors that contribute to an overall effect, roughly 80% of the effect comes from 20% of the causes.
Using a Pareto chart helps your team to prioritize and focus on patient safety interventions that have the greatest impact, thus saving effort and costs. This tool enables the team to make informed decisions and concentrate on the “vital few” (the factors that have the largest contribution to the effect). It also provides a rationale for not taking actions on the “useful many” (factors that have a relatively smaller contribution to the effect).
A Pareto chart is mainly used in the phase of problem identification. It presents the data in a visual manner and helps your team to communicate the problem or situation to senior management and seek their support or actions. Pareto chart is in a bar chart format in which the various factors that contribute to an overall effect are arranged in order from the largest to the smallest contribution to the effect.
In Conclusion
The above are the essential patient safety tools and techniques which are indispensable in healthcare. The toolkits can help you in identifying root causes, minimizing errors, and improving the overall quality of patient care. They can also bring sustained improvements by fostering a culture of safety and teamwork, enhancing communication, and proactively preventing failures. These toolkits are your essential companions in patient safety.
Download Patient Safety Toolkit Now
Unlock the potential for enhanced patient care with the QUASR Patient Safety Tools Templates – your ultimate resource for fortifying safety measures and promoting a culture of continuous improvement. Our carefully designed tools provide healthcare professionals with the means to proactively address risks, ensuring the highest standards of patient safety.
SBAR, Ishikawa Diagram and 5 Whys digital RCA tools, action tracking, workflow automation and alerts are part of QUASR system features. You can perform other patient safety techniques such as FMEA mentioned in this blog and attach the analysis in incident reports using the “Attachments” feature.
Start your 14-day free trial or get a demo of our premium software.






