What this Report is About
The World Health Organization recently published the Global Patient Safety Report 2024. The report provides a global perspective on patient safety implementation, in line with the Global Patient Safety Action Plan 2021–2030.
It has an in-depth analysis on how countries are addressing challenges and implementing actions to strengthen patient safety through multiple dimensions such as policies, strategies, regulations, international collaborations, clinical programmes, education, and more. The aim is to present a broad perspective on the state of patient safety on a global scale, highlighting both the progress made and persistent challenges and opportunities for improvement.
The report covers a comprehensive analysis of global patient safety efforts, including actions taken by countries, the burden of unsafe health care practices, case studies and comparative analyses.
This global report provides a vital resource of information for various stakeholders, including research institutions, health care organizations, industry players and advocacy groups. By providing insights into global patient safety strategies and identifying areas for improvement, it empowers stakeholders to drive positive change in healthcare safety and quality.
Below is an extract of the report’s summary findings. You may access the full report at this link: Global Patient Safety Report 2024.
Table of Contents
Summary of Findings
This global report explores the global patient safety situation, offering a comprehensive and detailed analysis of Member State survey data as well as other published sources. It presents a global overview, highlighting a wide range of patient safety initiatives and progress made around the world, in line with the strategic framework and suggested actions and its 7×5 matrix outlined in the Global patient safety action plan 2021–2030. The structure of the report directly aligns with the strategic objectives of the action plan, focusing on the implementation of strategies across nations to enhance patient safety.

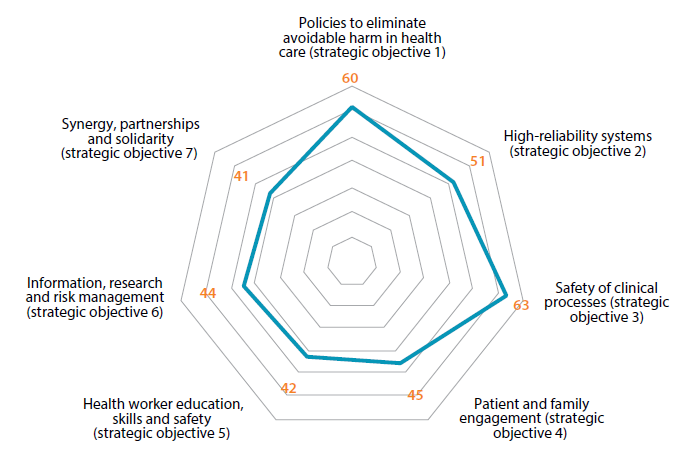
Strategic objective 1: Policies to eliminate avoidable harm in health care
- Although most countries recognize patient safety as a national health priority, only one third of countries have fully incorporated patient safety into their national strategies for achieving UHC.
- The development of policies, strategies, action plans, and programmes for patient safety is still in its early stages, and an even smaller fraction of countries report having adequate financial and human resources for implementation.
- Regulatory mechanisms such as mandatory licensing of health care facilities are widely used to enforce safety, with a significant number of countries enacting laws on the use of medical products and implemented the safety standards in health care facilities.
- World Patient Safety Day, established in 2019, has created unprecedented international momentum with 80% of Member States actively participating in annual campaigns and events to enhance awareness of patient safety.
- The WHO Global Patient Safety Challenges address critical risks to patient health and safety. Countries have taken actions on these initiatives, with almost 90% of countries addressing at least one of the challenges and one third of the countries implementing all the three challenges.
Strategic objective 2: High-reliability systems
- A safety culture in health care is recognized as crucial by most countries, yet only a quarter of countries reported to have made efforts towards developing a culture of safety in health care facilities and services.
- The WHO Global patient safety action plan 2021–2030 advocates for good governance in patient safety, with around half of the countries having designated national patient safety officers and establishing national coordination bodies.
- Although the significance of human factors in health care is increasingly being acknowledged globally, only around a quarter of countries have started to implement human factors principles in patient safety measures in clinical practice, use of medical devices, information technology solutions, and service delivery processes.
- A proactive and systematic approach to managing patient safety risks involves meticulous identification, examination and mitigation of potential hazards and risks in health care settings. Only a quarter of countries report implementation of risk management strategies and conduct regular mock drills.
- Most countries have established physical safety norms for health care infrastructure, but only about half report enforcing these norms, highlighting a gap between policy and practice in infrastructure safety.
Strategic objective 3: Safety of clinical processes
- Around 41% of countries have launched patient safety improvement programmes tailored to their specific contexts, addressing different sources of harm. Health care-associated infections and medication errors are prioritized in the majority of countries implementing such initiatives.
- Two thirds of countries have endorsed and are implementing the third WHO Global Patient Safety Challenge: Medication Without Harm. However, only a quarter of countries are actively addressing all three priority areas of the Challenge: high-risk situations, transitions of care, and polypharmacy.
- Around 60% of the countries report having a national programme for infection prevention and control, and half of the countries report implementing active surveillance systems for health care-associated infections.
- Countries have made significant investments in ensuring the safety of medical products. Almost all countries have functional pharmacovigilance programmes, nearly 80% have implemented blood safety programmes, and about half of the countries have initiatives for the safety of medical devices.
- Patient safety in primary and ambulatory care is less prioritized compared to safety in hospitals, with only 17% of countries systematically including safety in primary care programmes.
Strategic objective 4: Patient and family engagement
- Patients and their families are key partners in creating and executing policies and action plans for patient safety. However, only 13% of countries have appointed a patient representative to the governing board of the majority of their hospitals.
- Countries have recognized patient rights charters as a means of empowering patients, and around 70% of countries have either developed or are in the process of developing such charters at the national level.
- Collecting feedback from users on safety and service quality is a common practice for improving services. 80% of countries have mechanisms in place to gather such feedback, with nearly 20% also measuring patient reported care outcomes.
- Access to medical records is recognized as a key patient right. Around 80% of countries report having procedures in place for patients and families to access their medical records, although only 50% have taken proactive actions to inform patients about the procedures for accessing patients’ medical records.
- Health care organizations should have policies to promote transparency, including full disclosure if patients are harmed in health care. However, only a quarter of countries have established procedures for disclosing adverse events to patients and families.
- Increasing public awareness and education about patient safety is of paramount importance for making health care safer. While two thirds of countries have developed information and educational materials only 14 of countries have launched a focused campaign to provide information and education to patients and families for their involvement in self-care and empower them for shared decision-making.
Strategic objective 5: Health worker education, skills and safety
- Understanding of patient safety is essential for all health workers, yet comprehensive integration of patient safety in health professional education and training remains limited globally. Only around one fifth of countries have incorporated patient safety in their undergraduate and postgraduate professional education.
- While a quarter of countries provide specialized in-service training courses on patient safety, there is a significant global shortage of trainers on patient safety, with 14% of countries reporting sufficient training capacity.
- A quarter of countries have established patient safety competencies for all categories of health workers, and only in 14% of the countries core competencies for patient safety are incorporated in licensing and re-licensing requirements.
- There is a strong interdependence between patient safety and health worker safety that was highlighted during the COVID-19 pandemic, leading to increased national efforts in ensuring health workers’ health and safety. Around 70% of countries have established or are working towards establishing a national programme for occupational health and safety of health workers.
- While WHO recommends vaccination for all at-risk health workers, coverage of health workers against vaccine preventable diseases, as per the national immunization policy, is reported by nearly 55% of the countries.
Strategic objective 6: Information, research and risk management
- Although patient safety incident reporting and learning systems have been introduced in 70% of countries, their effectiveness remains limited, and only in one third of countries do the majority of health care facilities actively report safety incidents to these systems.
- Interoperability and international collaboration for sharing data between patient safety incidents reporting systems are limited, with only around one third of countries aligning their reporting formats with the WHO minimum information model.
- The implementation of electronic health records (EHR) in health care systems is increasingly recognized, with nearly 90% of countries reporting their adoption. However, full integration of EHR with health care processes is reported by only one quarter of countries.
- Three quarters of countries have identified patient safety indicators, yet only a minority integrate these into health information systems or publish annual safety reports, indicating a gap in data utilization for safety improvement.
- Research on patient safety remains a low priority, with only 11% of countries considering it a priority, although some integrate safety risk assessments in health technology evaluations.
Strategic objective 7: Synergy, partnerships and solidarity
- Enhancing patient safety and care quality through stakeholder engagement remains an evolving endeavour. Though around one-third of countries have identified key stakeholders, only 17% have implemented effective coordination mechanisms to fully engage these stakeholders.
- Professional associations and academic institutions are widely involved in patient safety efforts in most countries, indicating strong multisectoral collaboration.
- Countries are increasingly involved in global and multilateral discussions on patient safety, with around three quarters of countries participating in global ministerial summits on patient safety.
- Nearly 20% of countries report having established patient safety networks that facilitate programme coordination and sharing of best practices.
- Despite the growing recognition of the private sector as a key stakeholder in patient safety, there remains significant room for improvement in their involvement. While 65% of countries acknowledge private sector and industry as key stakeholders, only 12% actively engage them in their national patient safety initiatives.






