
Medication error – A leading cause of avoidable harm
Unsafe medication practices and medication errors are one of the leading causes of injury and preventable harm in healthcare systems across the world. Medication incident is also one of the most common patient safety incidents in healthcare settings.
Medication errors are costly in both human and economic terms. Globally, half of all avoidable harm in medical care is medication related, a quarter of which is severe or life-threatening. The cost associated with medication errors has been estimated at US$42 billion annually (source: World Health Organization).
Root causes of medication errors
Medication errors, near misses and adverse drug events occur at all phases of the medication use process – prescribing, dispensing, administering, and monitoring. Like other patient safety incidents, medication errors usually arise from poorly designed healthcare systems and products, as well as human factors such as fatigue, poor working environment, lack of communication, inadequate training, or staff shortages.
Other root causes are patient-related factors such as poor understanding on medication instructions. It could also be due to technology-related factors, such as electronic prescribing system not being used or implemented properly. Regardless, it is important to identify and address the root cause of errors to prevent future incidents and improve medication safety.
What can healthcare providers do to reduce medication-related incidents?
Medication error reduction strategies
Healthcare providers can consider the following initiatives and medication error reduction strategies:
Initiating a strong leadership to make medication safety a strategic priority.
Adopting practical tools and approaches to build safer processes and work practices.
Implementing a robust medication error reporting system.
Facilitating collaboration among interdisciplinary teams to analyse errors and identify root causes.
Adopting a proactive approach in risk identification.
Investing in technology such as barcoding and computerized physician order entry (CPOE) systems.
Engaging and educating patients about safe medication practices
A useful source of reference is California Medication Error Reduction Plan (CA MERP), a comprehensive framework and methodology to assess, improve, and evaluate medication safety.
Barriers to medication error reporting
One of the persistent issues facing healthcare providers is the under-reporting of medication incidents and near misses. Near misses, if unreported, can lead to actual medication incidents. Under-reporting means missed opportunities to identify system failures, learn from mistakes and take corrective actions to prevent future incidents.
There are numerous barriers to medication error reporting. Healthcare workers may be afraid to report because they fear punishment or retribution. Some may lack the safety awareness on the importance of incident and near miss reporting. Other barriers are heavy workload, burden of documentation, cumbersome reporting system, and lack of motivation to report as they don’t receive any feedback on the incidents they reported. These barriers and challenges apply to patient safety incident reporting in general. As medication errors are a major cause of injuries and harm to patients, there is a more urgent need to address medication error reporting.
Addressing these challenges requires a multi-faceted approach that includes creating a non-punitive reporting culture, educating healthcare workers about the importance of reporting errors, simplifying reporting processes, and providing adequate resources to support reporting and data analysis. A robust web-based medication error reporting system can solve some of challenges in reporting and managing medication errors.
Impact of a web-based reporting system
Findings from a study* on the impact of an online healthcare incident reporting software on medication error data collection are as follows:
- The number of documented medication errors increase by 132% after the web-based system was implemented.
- The number of intercepted errors increased from an average of 17.3% to 58.2%.
- Improved quality of reported data. Missing or unspecified data from cause-of-error variable decreased from 18.6% to 2.1%
- A significant shift in medication error culpability. Physician-attributed errors increased from an average of 4.8% to 27.5%, while reported errors attributed to nurses and pharmacists dropped from 92.5% to 70.1%.
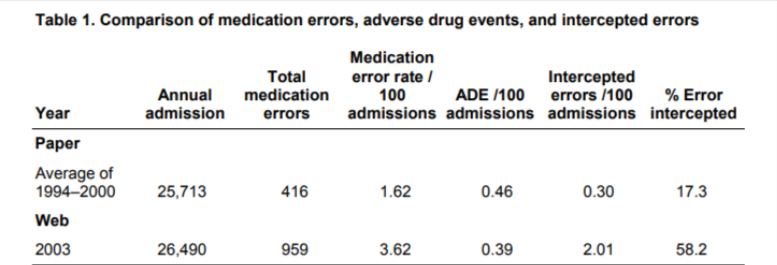
The study attributed the positive impact of a web-based reporting system to the system’s deliberate anonymity and ease of use, its ability to expedite reported medication error investigations, and the educational efforts directed at the creation of an open reporting environment.
*Source: “The Impact of a Web-based Reporting System on the Collection of Medication
Error Occurrence Data”. Authors: William J. Rudman, Jessica H. Bailey, Carol Hope, Paula Garrett, C. Andrew Brown.
What makes an effective web-based reporting system?
An effective medication error reporting system should address some of the barriers mentioned above, capture medication error-related data with proper categorization, facilitate investigation and root causes analysis, generate actionable insights, and track corrective actions.
Look for these features:
Easy to use web-based solution – A secure, web-based solution with user-friendly interface and role-based access. Users should be able to easily report medication errors and near misses using mobile devices. Keep the forms simple with guided questions and dropdown selections.
Option for anonymous reporting – Removing the fear of punitive actions will encourage more people to report medication errors and near misses.
Configurable forms – Flexible to configure forms to collect adequate information on medication errors. Easy to make changes to the forms as your organization’s practices mature or when new requirements arise.
Built-in best practices – Proper categorization of medication error related data such as patient outcome (ratings from Category A to Category I), product/drug information, type of medication error, causes of medication error and contribution factors. A good reference material is NCC MERP Taxonomy of Medication Errors.
Streamlined and automated workflow – A typical workflow involves incident notification, supervisor review, quality/risk review, investigation and RCA, and signoff. Process automation will enhance efficiency, communication and ensure a timelier incident closure.
Risk assessment – Conducting risk assessment will allow the quality and risk team to identify and prioritize high risk medication errors and near misses.
Investigation and RCA – Incorporating frameworks such as London Protocol into the system will ensure a comprehensive and thoughtful investigation and analysis. A reporting system that supports multiple incidents RCA will be particularly useful for the analysis of medication errors and near misses of similar nature/cause.
Action management – It is necessary to prioritize and assign corrective actions and recommendations after every investigation and RCA and monitor the actions to closure.
Communication and feedback – Allowing reporting persons to access and follow through on the incidents reported (except for sensitive cases) and view any improvement plans will encourage more reporting and wider participation to improve patient safety.
Reports and data analysis – Generating timely management reports with actionable insights.
In summary
Improving the effectiveness of medication error reporting requires leadership commitment to patient safety, along with strategies to reduce medication errors. A robust web-based reporting system that makes medication error reporting quick and easy, captures adequate data, and facilitates incident review to identify risks and root causes will enhance the effectiveness of medication error reporting. QUASR is a cloud-based incident reporting system that offers features described above.
Empowering Medication Error Reporting with QUASR
QUASR is a cloud-based healthcare incident reporting system. It offers functionalities that encourage ME reporting, facilitate collaboration, enable analysis, and track actions. QUASR’s ME form is designed in stepper form format with skip-logic condition, making it quick and easy to report MEs. The questions are based on guidelines and industry best practices on ME reporting. The form is easily configurable to meet specific requirements. Users are guided throughout the form to ensure all relevant data is entered. Click the link below to find out!
To view QUASR Medication Error Form and the complete incident reporting workflow in the system, click the link below to request free demo.






