In our previous blog, we discussed how polypharmacy significantly increases medication safety risk, especially in older people living with chronic diseases. In this blog, we will discuss how patient safety is compromised in transitions of care and what strategies must be adopted to overcome it.
Transitions of care is the patient’s movement from one healthcare setting to another or home. When patients receive care at various healthcare facilities, there is a greater chance of medication discrepancies, errors, and adverse drug reactions.
At each point in transitions of care, the medication a patient was taking prior to the transition needs to be identified by medication reconciliation. Medication reviews are vital at each transition to avoid or reduce medication discrepancies.
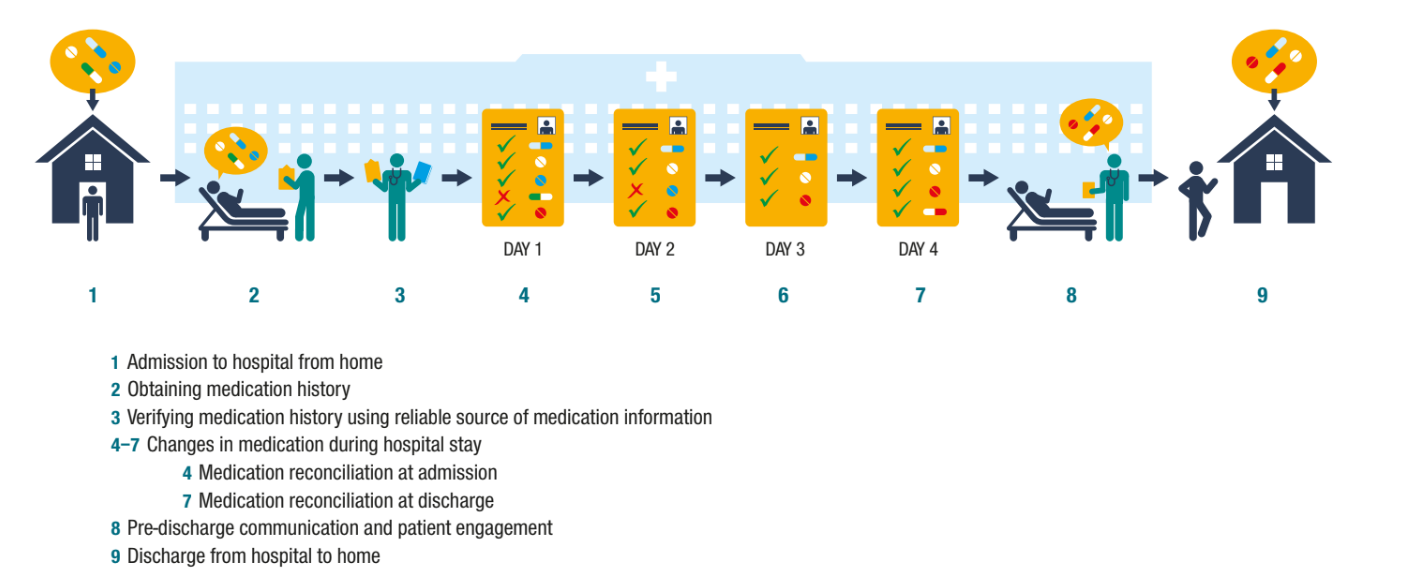
Image source: Medication Safety in Transition of Care by WHO
Table of Contents
Medication Harm Due to Discrepancies
Discrepancies or errors that are not identified and resolved may place the patient at risk of medication-related harm. For instance, adverse drug reactions often go unidentified or undiagnosed during routine clinical screening and treatment, which puts the patient at greater risk of further harm.
In addition, polypharmacy, high-risk medications, or the presence of morbidity increases the risk of a patient experiencing medication-related harm at any point during transitions of care settings.
Early confirmation of medication intake and timely diagnosis and management of medication-related harm is necessary to minimize patient harm. Reporting adverse drug reaction events to the patient safety incident reporting or pharmacovigilance systems is necessary to facilitate learning at organizational, national, and international levels.
Risks Associated with Insufficient Medication Safety
Medication-related harm affects almost every patient in the transition of care. The following are the risks associated with insufficient medication safety during transitions:
1. Medication errors
The risk of medication errors is potentially high during transitions of care. Such errors occur when a patient has been prescribed the wrong medication with the wrong dosage at the wrong time.
2. Medication duplication
Lack of communication between healthcare providers often causes medication duplication during transitions of care. When the patient is prescribed the same medication by multiple healthcare providers, it can lead to overdose or other adverse events.
3. Medication discrepancy
When patients are transferred from one healthcare setting to another, there is a high risk of medication discrepancy. The difference in medication regimen in new settings arises from poor communication, manual processes, patient forgetfulness, and time constraints. Medication discrepancies cause delays in treatment and increase potential harm to the patient.
Possible Barriers to Medication Safety
Challenges to medication safety in transitions of care are divided into three categories:
1. Patient level barriers
1.1 Competency
Competency refers to the patient’s understanding of the use of medications. Most patients don’t have enough knowledge on how to manage medications successfully.
Limited health literacy compromises the ability of patients to provide accurate medication histories at the time of hospital admission. Such inaccurate medication history leads to medication discrepancies.
Moreover, patients and family members also find it hard to understand the discharge instructions. It is because of their educational level, or they may be too reluctant to ask questions.
1.2 Insufficient engagement between patients, caregivers, and physicians
Lack of involvement of patients and caregivers with physicians during transitions compromises the quality of care. For instance, the patients and caregivers may not provide a comprehensive patient history to the physicians, which is necessary for making the right diagnosis. Additionally, they may not ask appropriate questions from healthcare practitioners regarding patient conditions.
Similarly, physicians may forget to provide adequate information on the patient’s condition and care, which leads to confusion and medication errors that put the patient at risk.
2. Health system-level barriers
2.1 Lengthy and confusing discharge paperwork
The lengthy discharge forms of hospitals complicate communication, decrease treatment compliance, increase the risk of discrepancies, and compromise patient safety. It is because written discharge instructions are long and hard for the patient and family to understand. Patients who don’t understand their medical discharge instructions will not stay compliant, which can lead to unfavorable outcomes.
2.2 Inadequate time to give health education
Limited time is another important system-level barrier. Generally, hospital staff doesn’t have sufficient time to thoroughly discuss discharge instructions with patients. When the staff cannot educate the patients, it causes confusion and compromises the quality of care.
2.3 Poor coordination between transitions
Poor communication and coordination between transitions of care negatively impact patient safety. It occurs when different practitioners and healthcare settings are not communicating or coordinating effectively to ensure continuity of care. This can result in medication errors, unnecessary treatments, adverse medication reactions, and other serious complications.
2.4 Inadequate Workforce
Lack of workforce in healthcare settings is another cause of compromised care during transitions. When healthcare providers are overloaded, they are not able to provide necessary care coordination and follow-up services for successful transitions of care. Moreover, chances for errors to occur are high, which can cause delays in diagnosis and treatment.
3. Practitioner level barrier
3.1 Lack of communication between physicians
Poor coordination and communication among healthcare providers are commonly seen in hospital setups. It is because different physicians visit at different times and add discharge orders without even interacting with each other. This inadequate transfer of information in transitions of care puts the patient’s safety at risk and compromises care.
3.2 Poor medication reconciliation
Poor medication reconciliation during transitions of care increases the risk of medication errors, medication duplication, delays in treatment, and increased healthcare costs. It usually occurs when healthcare providers are not aware of the complete and accurate medical regimen of the patient. And they end up prescribing medication that can lead to complications and hospital readmissions.
Potential Solutions for Ensuring Patient Safety in Transitions of Care
Optimizing patient safety as they navigate various healthcare settings is crucial.
The following strategies should be considered to optimize medication safety at transitions:
1. Improving information management
Effective information exchange is vital for patient safety. Healthcare facilities should improve the information management process by simplifying discharge forms and introducing e-script. For instance, the discharge forms should be very simple, written in lay terminology, and organized with separate categories so the patients can easily read and understand the information. Similarly, the use of e-scripts should be established to overcome meditation discrepancies. When electronic prescriptions are sent to pharmacies, it will reduce the risk of medication harm.
Health systems should switch to centralized electronic health records (EHRs) for a long-term change. It keeps the physicians connected, allows seamless transfer of information, and minimizes the risk of errors at transitions of caregivers.
2. Medication reconciliation
Healthcare professionals should be trained for proper medical reconciliation. In this process, healthcare professionals work closely with patients and their family members to ensure that complete and accurate information is transferred consistently across care transitions.
Effective medication reconciliation allows caregivers to avoid hazardous drug combinations, dose changes, duplications, and adverse events. It also reduces its reliance on patients’ recall abilities and allows easy analysis of medication information for better management decisions.
3. Increase engagement between patients, caregivers, and physicians
Improved communication between patients, caregivers, and physicians is critical for reducing the risk of adverse events.
Healthcare professionals should fully inform the patients and caregivers about the patient’s condition, treatment options, and expected outcomes. When the healthcare team involves patients and caregivers in the treatment process, it develops trust and makes it easier for them to communicate. As a result, they are more likely to follow the treatment plan as prescribed.
4. Incorporating an incident reporting system
Healthcare facilities should set up an incident reporting system to ensure patient safety during transitions of care. It is designed to strengthen existing organizational processes by automating incident management workflow, performing risk assessment, providing real-time analytics and insights, and resolving incidents related to patient care.
The incident reporting system allows healthcare providers and organizations to track and report incidents related to patient care during transitions and enables them to take proactive steps to address the issue before it results in adverse events. It also helps identify areas that require improvement to ensure better patient outcomes and increased efficiency in transitions of care.
By incorporating an incident reporting system, providers can provide valuable information that can be used to identify patterns or common causes of medication errors.
It also allows for:
- ● Early identification of potential safety issues: Through a reporting system, healthcare professionals can identify the possible issue and risk factors leading to medication errors. It enables them to take quick actions to avoid future errors and ensure patient safety.
- ● Root cause analysis: Incident reporting systems work efficiently for conducting root analysis of the underlying cause of medication-related errors. This information helps in making targeted interventions to prevent future events which put the patient at risk.
- ● Quality improvement: With incident reporting systems, healthcare providers can get instant reports on their performance aimed at improving medication safety. It allows them to track their interventions’ effectiveness, evaluate their efforts’ impact, and make adjustments as needed.
- ● Compliance: Incident reporting systems can be used to demonstrate compliance with regulatory requirements related to medication safety, such as The Joint Commission’s National Patient Safety Goals.
- ● Early identification of potential safety issues: Through a reporting system, healthcare professionals can identify the possible issue and risk factors leading to medication errors. It enables them to take quick actions to avoid future errors and ensure patient safety.
5. Improve coordination between different transitions of care
Coordination between transitions of care is essential for positive health outcomes of patients. It eliminates the risk of medication errors, discrepancies, and adverse events. When patients receive consistent and appropriate care throughout different stages of healthcare, it can prevent hospital readmissions and unnecessary treatments. So, physicians, specialists, nurses, and other healthcare professionals should work together to provide comprehensive and coordinated care to patients.
6. Workforce planning
Effective workforce planning is critical for the quality of care of patients. When there is adequate staff during different stages of the healthcare journey, the patients will receive appropriate and consistent care. This results in better treatment and reduced medical costs. So, healthcare settings must identify the number of healthcare staff required to meet the demands of patients.
Conclusion
Patient safety during transitions of care is a critical concern for the healthcare industry. To overcome this challenge, a multi-faceted approach is required where organizations, practitioners, and patients must work together to ensure smooth transitions. Healthcare organizations should optimize and establish clear protocols for medication management to avoid medication-related harm. An electronic system must be incorporated to improve communication among patients and care providers.
Additionally, patients should be educated about their rights and responsibilities toward their medications. All these approaches will help to reduce the risk of medication errors and improve patient outcomes.
Are you planning to incorporate an online incident reporting system to improve patient care? QUASR is a robust incident reporting system, which makes it easier for healthcare settings to identify, investigate, and manage risks by implementing corrective actions.
Book a demo to learn more about medication reporting in QUASR.
Empowering Medication Error Reporting with QUASR
QUASR is a cloud-based healthcare incident reporting system. It offers functionalities that encourage ME reporting, facilitate collaboration, enable analysis, and track actions. QUASR’s ME form is designed in stepper form format with skip-logic condition, making it quick and easy to report MEs. The questions are based on guidelines and industry best practices on ME reporting. The form is easily configurable to meet specific requirements. Users are guided throughout the form to ensure all relevant data is entered. Click the link below to find out!
To view QUASR Medication Error Form and the complete incident reporting workflow in the system, click the link below to request free demo.






