
Healthcare Quality
Under-reporting Patient Safety Incidents: A Real Problem
Under-reporting is a critical issue that should be analyzed and treated by the hospitals on priority. Learn more about under-reporting here.

Under-reporting is a critical issue that should be analyzed and treated by the hospitals on priority. Learn more about under-reporting here.
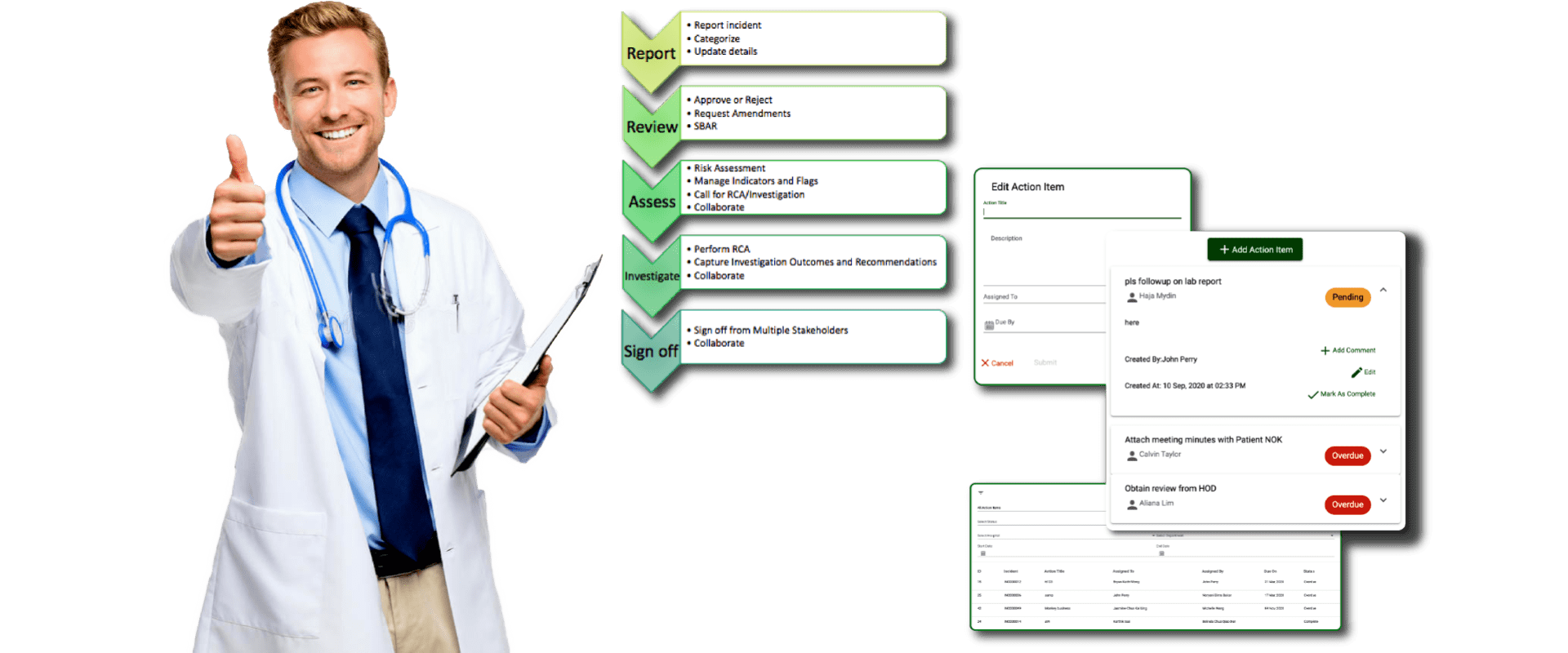
In this post, allow us to introduce QUASR Basic to you. How it is different from Lite, what more does it offer, and how it can fit well in your process