
Unlocking Success: The Power of Staff Participation in Incident Management
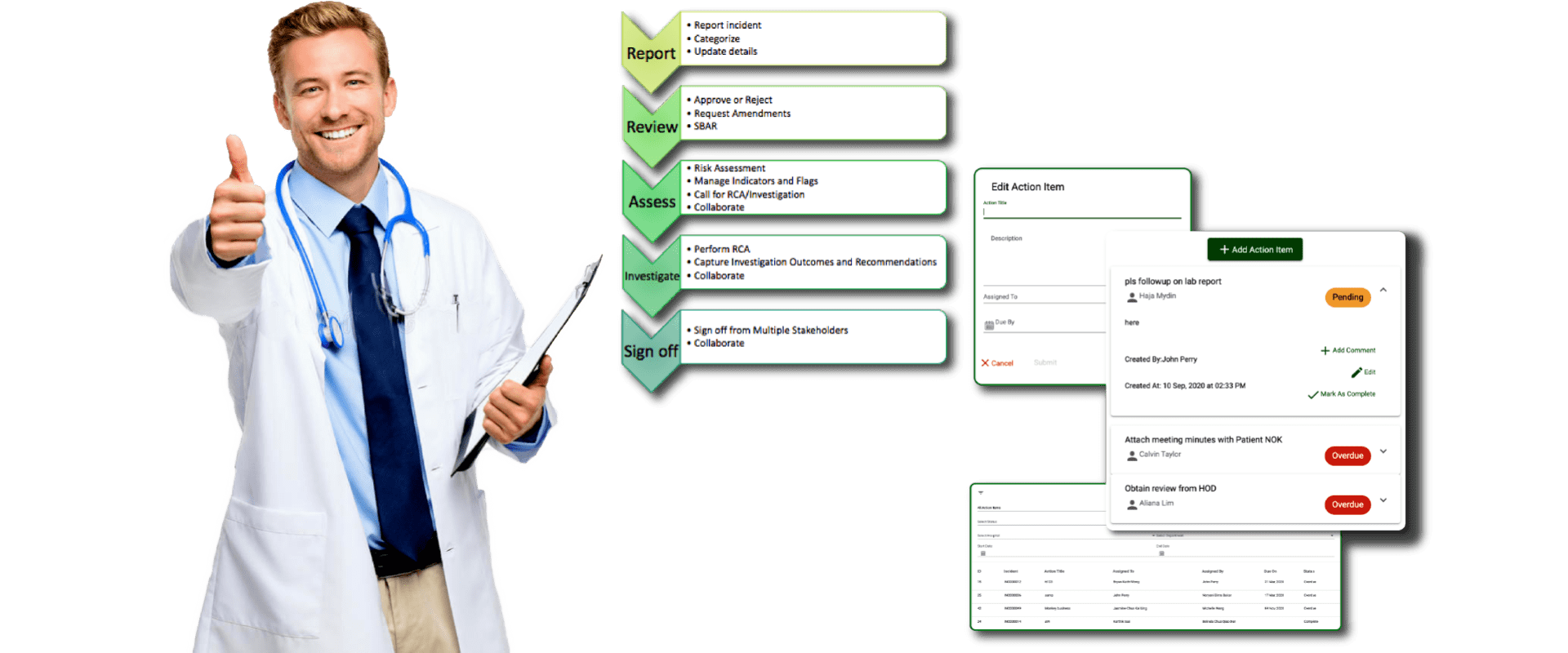
Active participation is an essential ingredient of all successful systems. Incident or Risk management is no exception to this.

Active participation is an essential ingredient of all successful systems. Incident or Risk management is no exception to this.

Anonymous reporting is when an incident report is not attached to any particular user/staff in the system. Learn more about this feature.

Sensitive Incidents are the digital equivalent of a “Private & Confidential” document of the paper-office era. Learn more about this feature.

Over the last decade or more, some successful maneuvers facilitated by the aviation industry have considerably reduced the risk of accidents and calamities.

This is a complete guide to incident reporting in healthcare in 2021. Learn about the purpose of incidents reports, types, and much more.
In this post, allow us to introduce QUASR Basic to you. How it is different from Lite, what more does it offer, and how it can fit well in your process

When you have a legacy system and are looking to keep the same process in your digital system, Or when you want to map your existing manual process as-is into the new system – Both these approaches, frankly, are inefficient
QUASR Lite is an online incident repository for hospitals. It is a simple data capture tool and allows you to capture the incident data in a structured format. It makes your life easy to gather incident statistics and generate reports.
WHO designated 17 September World Patient Safety Day theme as “Health Worker Safety: A Priority for Patient Safety”.