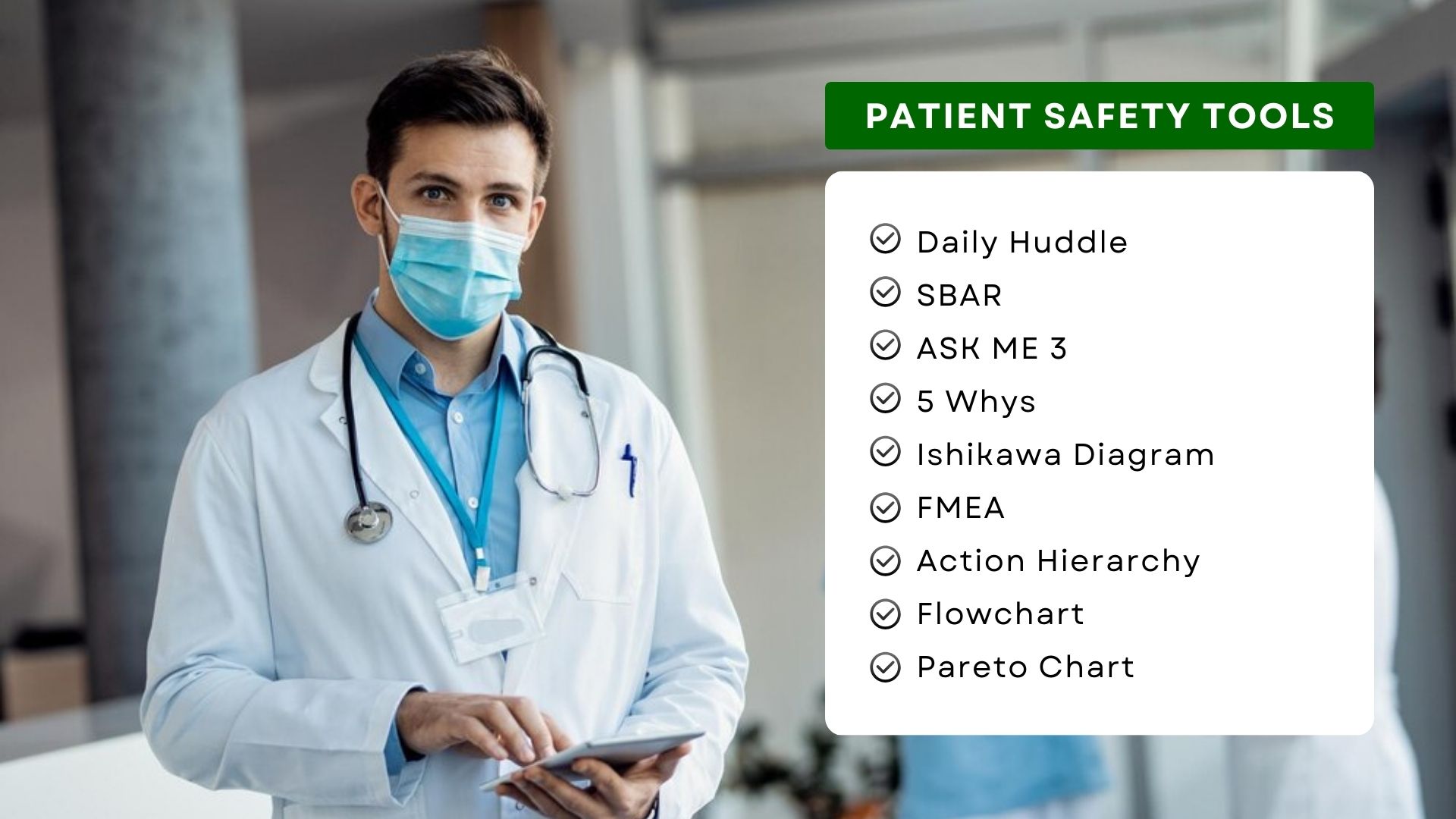
9 Essential Patient Safety Tools For Quality Improvement in Healthcare
Simple and easy-to-use tools can bring surprising insights and results. Most healthcare professionals, especially safety and quality officers, are familiar with and use them during their day-to-day work. Yes, we are talking about essential patient safety tools and techniques that you use to ensure the delivery of safe and reliable care. These tools are indispensable for safety and quality management in healthcare.